Personalised Care and Support Planning: 'What matters to you?'
Personalised Care and Support Planning is an umbrella term that covers the planning approaches that teams, services and organisations use to have ‘What matters to you?' conversations with people.
‘What matters to you’ conversations are recorded in a Personalised Care and Support Plan (PCSP) and should be seen as the first chapter in someone's ‘book’.
People with a number of long-term conditions often have a range of treatment and care plans that are additional chapters in their ‘book’ and should be viewed alongside their PCSP.
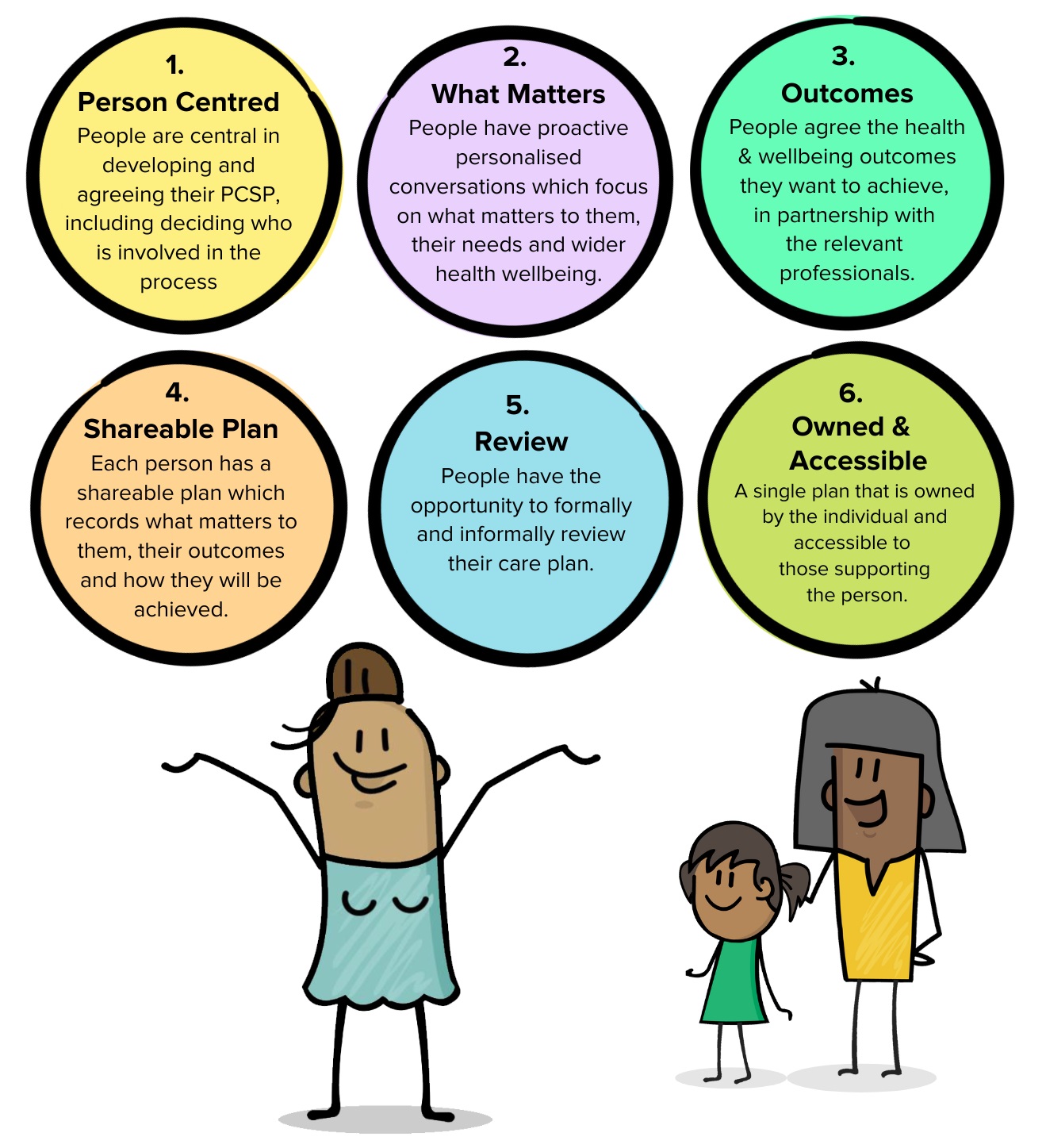
All Personalised Care and Support Plans must be aligned with the national criteria, as described in the illustration below:
Always be relevant
As a person's life progresses, their 'chapters' and needs will evolve and change. Their personalised care and support plans need to evolve and change with them. It's important that a person's support circle is aware of these changes to make sure that the support given is relevant to the care they need.
The document below is a What Matters To Me plan, which is an example of a personalised care and support plan:
| Thumbnail | Title | Size |
|---|---|---|
| folder icon | Peoples Stories Template | |
| folder icon | Co-Production | |
| My Personalised Care and Support Plan | 184.20 KB |
Please click on the sections below for more information.
Matt Evans chatted to Vicky Martin about the quality assurance process undertaken in the Stroke Service and what impact that is having as they develop a more personalised approach to care and support planning.
FAQs
Personalised Care and Support Planning
Frequently Asked Questions
What is Personalised Care and Support Planning?
Personalised Care and Support Planning is an umbrella term that covers the planning approaches that teams, services and organisations use to have ‘What matters to you?' conversations with people.
‘What matters to you’ conversations are recorded in a personalised care and support plan and should be seen as the first chapter in someone's ‘book’.
People with a number of long-term conditions often have a range of treatment and care plans that are additional chapters in their ‘book’ and should be viewed alongside their personalised care and support plan.
What is the difference between Personalised Care and Support Planning and Personalised Care and Support Plans
Personalised care and support planning is a series of conversations in which the person actively participates in exploring their health and wellbeing, within the context of their whole life and family situation. It ensures a better or different conversation between a person and the practitioner to create a more equal relationship. Personalised Care and Support Planning is an umbrella term that covers the various personalised care plans in place across the spectrum of teams and organisations.
A personalised care and support plan is developed following an holistic conversation around the person about their health and wellbeing needs. The person, or their family, work hand-in-hand with their professionals to co-produce an agreed personalised care and support plan. Not to be confused with a treatment plan or a detailed assessment.
There is no set template for what a plan should look like, but it should reflect the following:
- a way of capturing and recording conversations, decisions and agreed outcomes in a way that makes sense to the person.
- should be proportionate, flexible and coordinated and adaptable to a person’s health condition, situation and care and support needs.
- should include a description of the person, what matters to them and all the necessary elements that would make the plan achievable and effective.
To count as a personalised care and support plan it must meet the 6 criteria below:
Person-centered – People are central in developing and agreeing their PCSP including deciding who is involved in the process.
What matters – People have proactive, personalised conversations which focus on what matters to them, their needs and wider health wellbeing.
Outcomes – People agree the health and wellbeing outcomes they want to achieve, in partnership with the relevant professionals.
Shareable Plan – Each person has a shareable plan which records what matters to them, their outcomes and how they will be achieved.
Review – People have the opportunity to formally and informally review their care plan.
Owned & Accessible – A single plan that is owned by the individual and accessible to those supporting the person.
What makes a good, personalised care and support plan?
A good, personalised care and support plan:
- is a way of capturing and recording conversations, decisions and agreed outcomes in a way that makes sense to the person.
- should be proportionate, flexible and coordinated and adaptable to a person’s health condition, situation and care and support needs.
- should include a description of the person, what matters to them and all the necessary elements that would make the plan achievable and effective.
Who needs personalised care and support planning?
Personalised care and support planning can be beneficial to anyone with ongoing care needs or long-term conditions. It provides an opportunity to discuss what matters to the person, the outcomes they want to achieve, and what support they can access, whether through statutory services or through personal connections and local Voluntary, Community and Social Enterprise services, to help them build their knowledge, skills and confidence to manage their health and wellbeing.
The complexity of a person’s needs, the number of conditions they manage, the breadth of services they are currently accessing, and their preferences will influence the type of support they might receive and the level of choice and control they have when managing their health and care. This ranges from being signposted to support to self-care, to people having control over their care package using a personal health budget or integrated personal budget. At the heart of these different levels of support is a personalised conversation based on what matters to them.
What are the benefits of doing a personalised care and support plan?
Valuing people as active participants and experts in the planning of their own health and wellbeing ensures they are in the driving seat of decision making and that the outcomes and solutions developed have meaning to the person in the context of their whole life. This leads to improved chances of successfully supporting them.
A personalised care and support planning means the person will not have to repeatedly share their story time and time again. They will have a series of conversations that result in a single integrated personalised care and support plan.
How does this affect my patients/the people I support?
Personalised care and support planning is likely to have the following impact on people and their families, carers:
- People will have a different or better conversation with practitioners which focuses on what matters to them and what is working and not working in their life.
- This will be done in a way that builds on their skills, knowledge and confidence.
- People will experience an integrated process coordinated by a single, named coordinator and a single care and support plan developed in partnership and owned by them.
- People will have the chance to regularly review their care and support plan.
- It’s easy to find out what support and services are available
What is the long-term NHS goal of PCSP?
Personalised care and support planning has been an integral part of social care and voluntary, community and social enterprise (VCSE) sector for many years and getting it right has been essential for people to gain more choice and control over their life and the support they are receiving. This is now recognised by the NHS as critical part of being able to embed personalised care and has been included as one of the key components of the universal personalised care model.
Will I be given a printed copy of the staff Personalised Care and Support Planning Information Booklet?
At the moment the booklet will be available for everyone online. This means you can download and print if you wanted or download and save to your own files.
The information about Personalised Care and Support Planning talks about it being the first chapter of someone’s book. Is there an actual book for us to record it in?
No, it should be recorded digitally.
Is Personalised Care and Support Planning applicable in the Voluntary sector?
Yes
What is the Care Portal?
The Lincolnshire Care Portal is a secure computer system that enables staff members, across all partner organisations in Acute, Community, Primary, Social & Mental Health Care settings to view an integrated care record for patients. It brings together selected patient information from multiple organisations and systems in real time. As patient data is included from all partner organisations (LCHS, LPFT, ULHT, Primary Care (GP Record), LCC Mosaic Social Care information, it is truly a single source system that has a wealth of patient data and a Care Plan capability.
As a system we need to transition to one digital care plan solution that works alongside an individual’s Shared Care Record, which the Care Portal provides. As staff across all partner organisations have access to the Care Portal, we need to transition to this single shared care plan solution to avoid duplicating effort by adding the same details to another system. It’s important to focus on the benefits of having a Shared Care Record that has patient data from all partner organisations and that facilitates a Care Plan that works alongside that record.
The What Matters to Me Care Plan is about what is important to the person, not a summary of their health conditions. The Care Plan focuses on the important details as their patient data and history is already in the Shared Care Record. To date we have over 2000 individual care plans that have been added to patient records using the Care Portal. There are e-learning modules available to learn more about the Care Portal, click here to access this along with hints and tips on how to get the most out of this digital solution.
I don’t have access to the Care Portal, how do I get it?
GP Practice staff:
Your Practice Manager is responsible for raising the access request by emailing lccg.stpdigital@nhs.net. The email needs to be clearly labelled “Care Portal Access” followed by the practice name (ie. Care Portal Access – Sleaford Medical Group). The Practice Manager will need to include the practice’s Care Portal Access Spreadsheet’ with all fields completed for the staff member requesting access, including Practice ODS Code etc. (if your practice manager does not have your practice spreadsheet, they will need to email (lccg.stpdigital@nhs.net) and request a copy be sent)
PCN Employed staff:
You need to contact your Single Point of Contact (SPOC) for access - this will usually be your PCN Lead or Practice Manager. Your SPOC is responsible for managing staff access requests by following agreed processes using standardised templates (as above)LCC and St Barnabas staff:
You will need to contact the Council’s Single Point of Contact for access. Your SPOC is responsible for managing staff access request by following agreed processes using standardised templates (as above.)
ULHT, LCHS and LPFT
Each organisation has their own Digital Team that manage access to systems including the Care Portal and is responsible for allocating the appropriate Role Based Access Control (RBAC) to their staff members. To request access, please contact your organisation’s Digital Team.
Why should I add the plan I have developed with the person to the Care Portal?
The Care Portal is fed by source data from all partner organisations and is the primary digital tool. Once a Care Plan is added to a patients record ALL health & social care staff members can see and contribute to that single shared care plan.
Can everyone access plans on the Care Portal? Who are the partner organisations?
All partner organisations can access the Care Portal. This includes ULHT, LCHS, LPFT, NWAFT (for those patients that have attended Peterborough Hospital), Lincolnshire County Council, Adult Social Care, GP Practices and Primary Care Networks. Other patient data feeds are received from Whzan, EPaCCs and East Midlands Ambulance Service. Work is in progress to bring the voluntary sector organisations on board so they can access the Care Portal, where it is recognised that they work collaboratively. Below are two visuals that show all the organisations that can access the Care Portal and what organisational patient data is presented in the Care Portal.
We use SystmOne/RIO/MOSAIC .. why do I have to use the Care Portal as well?
Having everyone use a single system for Care Plans saves staff having to log into multiple other systems. The key requirement is to have a Single Shared Care Plan that staff members, regardless of which organisation they worked for were able to add, edit and contribute to. Any changes made to a patients Care Plan are tracked which means no data is ever lost. You can also see who has contributed to the single shared care plan, which is useful should you need to speak with colleagues about the individuals care and support. Rigorous testing has proved that staff across each partner organisation can access the same care plan electronically and no data is lost. The care portal has full version control, so all previous care plans are visible so you can see the changes and when they are made over the care plan’s lifetime.
It’s duplicating and time consuming as I already do assessments in SystmOne or RiO etc?
A personalised care and support plan isn’t the same as an assessment. It’s a summary of a person’s health and social care history over time. Because the assessment data in a person’s health and social care information is also available in the Shared Care Record, this means you don’t have to replicate this information – staff members can see the patients details and focus on the care plan content to learn what is important to the individual and how best they can be supported.
We already do holistic assessments, are these a type of Personalised Care and Support Plan?
No, a personalised care and support plan is developed following an holistic assessment around the person about their health and wellbeing needs. It’s about a series of conversations that captures a summary of a person’s health and social care history over time.
See What makes a personalised care and support plan
How do I know if the care plan that we use counts as a Personalised Care and Support Plan?
To align with personalised care and support planning, the plan must meet the 6 criteria – see matrix below.
I’ve done an Advance Care Plan with my patient. Do they also need a Personalised Care and Support Plan?
No, if your Advance Care Plan meets the NHSE/I criteria and it therefore counts as a Personalised Care and Support Plan. Click here to read the universal principles for an Advance Care Plan. Personalised Care and Support Planning is an umbrella term that covers the various personalised care plans in place across the spectrum of teams and organisations
Does a good quality ReSPECT form count as a Personalised Care and Support Plan?
No, a ReSPECT form is a plan which details a person’s wishes in the case of an emergency when they may not be able to express that themselves. It is not a personalised care and support plan.
Does a Cancer Holistic Needs Assessment (HNA) count as a Personalised Care and Support Plan?
Yes, a Cancer Holistic Needs Assessment meets the NHSE/I criteria and therefore counts as a personalised care and support plan.
Does the IROC/HOPE conversation count as a PCSP?
Yes
What is the difference between a Personalised Care and Support Plan and a What Matters To Me Plan?
A What Matters to Me plan is a Personalised Care and Support Plan
Why can’t we complete PCSP on paper like we’ve always done?
You can, but please be mindful this makes it difficult for others to see the content and will require communication with colleagues (usually via email) which isn’t the most secure method. Having this stored on an electronic system (Shared Care Record) allows all other professionals across Lincolnshire to access the same information without having to email individuals and waiting for responses. It avoids having to make an individual repeat the same conversations time and time again and reduces the risk of things being missed or forgotten in those repeated conversations. If the individuals’ personalised care and support plan changes in any way, its then immediately available for others to see – this saves you having to send out an updated paper version to everyone involved in that person’s care and support.
Why is it better to complete a PCSP on the Care Portal as opposed to SystmOne?
There is an expectation that professionals / practitioners across Lincolnshire who work in all of the health and care settings, benefit from and use the same system. Having a personalised care and support plan that works alongside the Shared Care Record in the Care Portal allows all users to see important health and social care information in one place – which means you shouldn’t have to log in and out of different systems to build a picture of the individual. The Care Portal’s planning capability has full audit history that includes the names, dates and times of any changes made to that person’s plan. Below provides a visual for all the different organisations that can access the Care Portal.
How does this affect what I already do?
This will be different for everyone. Some of you are already having these conversations so the way you work won’t be that greatly affected. However, those just moving into this way of working will feel a bigger impact affecting the way they do things. It’s imperative the shift happens to benefit not only the workforce but the people of Lincolnshire.
How will this impact the person’s outcomes?
Personalised care and support planning is likely to have the following impact on people and their families, carers:
- People will have a different or better conversation with practitioners which focuses on what matters to them and what is working and not working in their life.
- This will be done in a way that builds on their skills, knowledge and confidence.
- People will experience an integrated process coordinated by a single, named coordinator and a single care and support plan developed in partnership and owned by them.
- People will have the chance to regularly review their care and support plan.
- It’s easy to find out what support and services are available
How can PCSPs be shared with the VCSE organisations if requested by the patient?
We are working to give VCSE organisations access to the care portal. Whilst this is not in place yet, we recommend you encourage the person who owns the plan (the patient) to share it with them as it is their plan.
Is there any training around PSCP conversations that I/my team can access to shift the focus of the conversation?
Yes, practitioners can sign up for personalised care and support planning training in the Learning and Development section of this site.
Is there an example of a What Matters to Me template that I can look at?
Key standards
NHS England (remove - and Improvement) have also worked with partners to co-produce a six-step criteria which must be used to demonstrate that the conversations and plans are of a high standard.
All six of these criteria need to be in place for it to meet the standards for a personalised care and support plan.
- People are central in developing and agreeing their personalised care and support plan including deciding who is involved in the process.
- People have proactive, personalised conversations which focus on what matters to them, paying attention to their needs and wider health and wellbeing.
- People agree the health and wellbeing outcomes they want to achieve, in partnership with the relevant professionals
- Each person has a sharable personalised care and support plan which records what matters to them, their outcomes and how they will be achieved.
- People have the opportunity to formally and informally review their care plan.
- People have a single plan that is owned by the individual and accessible to those supporting the person.
Family and carers are also considered as an important part of this process, where appropriate. Informal carers may also require their own personalised care and support plan.
Here is a tool you can use to ensure your Personalised Care and Support planning conversations and plans meet the criteria Personalised Care and Support Planning (PCSP) Quality Framework Document
What we want to achieve
As a Lincolnshire integrated care system we want to see personalised care and support planning embedded as a way of working across all services. This means:
- Staff being able to access a range of learning and development approaches which focus on personalised conversations.
- Embedding the five key standards in care and support planning approaches and creating an effective and meaningful quality assurance processes, which include people with lived experience.
- Agreeing a methodology for reporting personalised care and support plans.
How will we get there?
We have already taken learning from other service areas and parts of the system who have already implemented personalised care and support planning, including learning disabilities, maternity and adult and children’s social care.Using continuous improvement methodology we are now trying out the approach in specific place based teams and service area to understand how this could work in different areas. This allows as many people as possible to get involved in helping design and shape collectively how these plans become a useful tool for everyone.
What we have done so far
Co-production
Working with people with lived experience we have co-designed a template for a ‘What matters to me? plan’. This documents have been produced to make them as simple and easy to use as possible.
Developing the digital record
As part of work to develop a central Lincolnshire Care Portal we have launched online care planning tools, which enable practitioners to create and start to populate care plans or contribute to existing plans. This enables one digital plan to be shared with the relevant people who have access to the Care Portal.
Lincolnshire conversation
We are initially rolling out the ‘Lincolnshire conversation’ in adult care services at Lincolnshire County Council.
Learning and development programme
We have commissioned EveryOne, a local charity who have a real passion for person centred care, to deliver Personalised Care and Support Planning training for practitioners in Lincolnshire. This training includes a more detailed look at why it is important to understand what matters to people, the tools we can use for these conversations, and how we can support people to stay at the centre of their care.
The feedback we have received regarding this course has included:
"This approach actually works. It’s an efficient use of time and is much more rewarding. By finding out what’s important to the patient it gets them on the same page as you and stops all the argy bargy.”
Occupational therapist at United Lincolnshire Hospitals NHS Trust
Resources
Introduction for Healthcare professionals booklet on Personalised Care and Support Planning
Introduction for Healthcare professionals PowerPoint on Personalised Care and Support Planning
Here is a tool you can use to ensure your Personalised Care and Support planning conversations and plans meet the criteria Personalised Care and Support Planning (PCSP) Quality Framework Document